Background
The emergency resuscitative thoracotomy (RT), aka The ED Thoracotomy, is a procedure performed as a last-ditch effort during resuscitation of a patient in traumatic arrest or impending traumatic arrest. Unfortunately despite physicians’ best efforts, outcomes for this procedure are generally poor. The largest review of outcomes after RT performed in the emergency department found an overall survival of 7.4% (8.8% for penetrating injury, 1.4% for blunt injury), with good neurological outcomes present in 92.4% of surviving patients [2]. Furthermore, given the lack of high quality evidence on this procedure, there are no universal guidelines that exist to determine optimal candidates [3,4]. Point-of-care ultrasound has become a core adjunct in evaluation of the trauma patient, however there is minimal data evaluating its utility in determining which trauma patients may benefit from RT [5].
FAST Ultrasound Examination as a Predictor of Outcomes After Resuscitative Thoracotomy: A Prospective Evaluation
Clinical Question
Can the Focused Assessment Using Sonography for Trauma (FAST) predict survival after a RT in patients presenting to the emergency department in traumatic cardiac arrest?
Methods & Study Design
- Population
- All penetrating trauma patients with absent vital signs and blunt trauma patients with a loss of vital signs en route or in the resuscitation bay that underwent RT.
- Intervention
- A FAST exam was performed just prior to RT to assess for the presence or absence of a pericardial effusion and cardiac motion.
- Outcomes
- Survival to Discharge or Organ Donation
- Design
- Prospective, observational study performed at a single academic level-1 trauma center
- Excluded
- Patients who were taken directly to the OR for an emergent or urgent thoracotomy were excluded.
- Patients who did not have a FAST exam performed prior to RT were excluded from analysis
Results
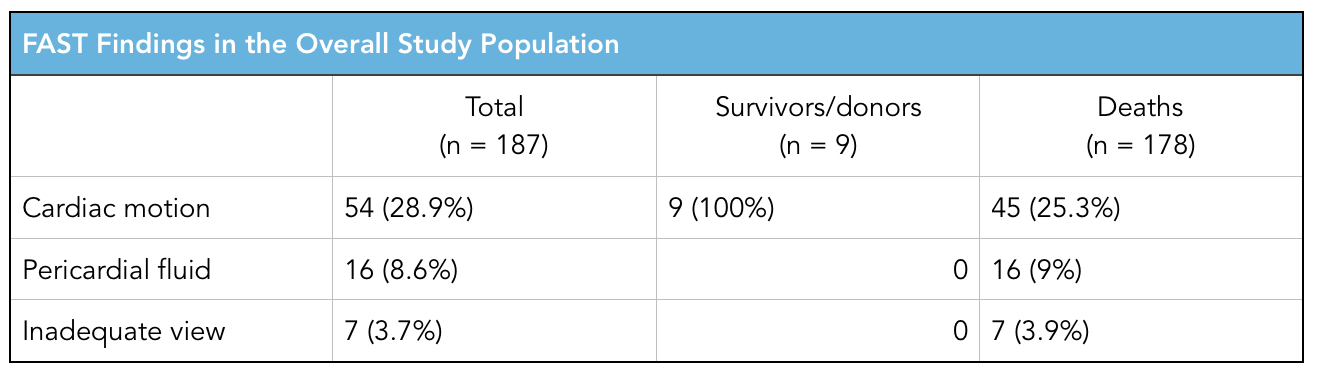
-
- 223 patients underwent RT, 187 underwent analysis (36 had no FAST performed)
- Primary Outcome
- Survival: 3.2%
- Organ Donation: 1.6%
- Primary Outcome
- 223 patients underwent RT, 187 underwent analysis (36 had no FAST performed)
Strengths & Limitations
- Strengths
- First large, prospective observation study on emergency RT
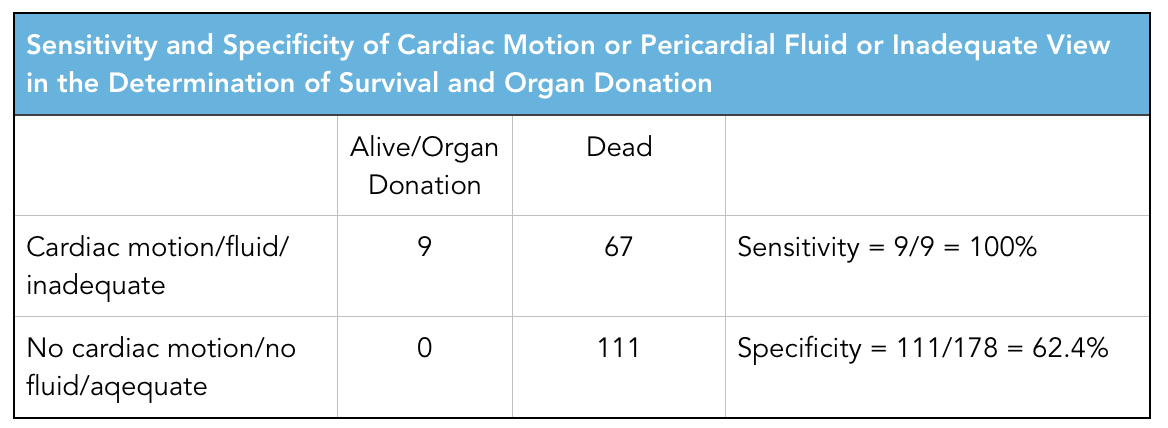
- Sensitivity analysis performed to include patients who had inadequate views obtained
- Limitations
- Study performed at a high-volume, single academic level-1 trauma center with which may skew generalizability
- Residents who had formal training in the FAST exam performed all ultrasound scans. Many emergency medicine physicians are not credentialed in ultrasound or FAST examination
Author's Conclusions
"In summary, for the patients that arrived to hospital and underwent a FAST examination, all survivors and organ donors had visible cardiac motion. If no cardiac motion or pericardial effusion was seen, the survival was zero. Ultrasound was, therefore, able to effectively identify those patients who had the potential to survive the RT and discriminate them from those who did not. Utilizing ultrasound would have resulted in the avoidance of a significant proportion of thoracotomies which were ultimately found to be futile.”
Our Conclusions
This is a well done study examining the utility of the FAST exam in identifying which patients will potentially benefit from emergency RT. One may look at the primary outcomes of this study and think that the very low overall survival rate (3.2%) does not jive with previously reported studies. However, it is important to note that during the study period, 21 patients who had a penetrating cardiac injury and went straight to the OR for thoracotomy, were excluded. All of these patients survived. If we were to incorporate this number into the the final analysis, survival would be ~13% which fits better with previous data. But that isn’t the point of this study. The big question that I feel is appropriately answered is which patient population can we safely avoid undertaking an emergency RT, knowing it is futile. While resource utilization for a procedure of this magnitude may be less burdensome at an academic level-1 trauma center, performing a RT in an emergency department where this is rare occurrence requires a much larger undertaking by the staff. The new data from this study, demonstrates that patients who did not have cardiac motion or a pericardial effusion on initial FAST had a zero survival rate. This is practice changing, especially for providers who rarely perform this procedure. If an experienced trauma team performing this procedure had zero survival rate in patients with no cardiac motion or pericardial effusion, it is safe to say that a provider with less experience will not perform better. Furthermore, having real time data to share with the entire resuscitation team during a traumatic arrest can provide closure to the team and a sense that performing any further heroic procedures is futile.
The Bottom Line
The FAST exam is a critical adjunct in traumatic patients and should be applied to all cases of traumatic arrest in order to determine the utility of performing an emergency RT.
References
-
- Inaba K, e. (2017). FAST ultrasound examination as a predictor of outcomes after resuscitative thoracotomy: a prospective evaluation. - PubMed - NCBI . Ncbi.nlm.nih.gov. Retrieved 4 July 2017, from https://www.ncbi.nlm.nih.gov/pubmed/26258320
- Rhee PM, e. (2017). Survival after emergency department thoracotomy: review of published data from the past 25 years. - PubMed - NCBI . Ncbi.nlm.nih.gov. Retrieved 4 July 2017, from https://www.ncbi.nlm.nih.gov/pubmed/10703853
- Seamon MJ, e. (2017). An evidence-based approach to patient selection for emergency department thoracotomy: A practice management guideline from the Eastern Association ... - PubMed - NCBI . Ncbi.nlm.nih.gov. Retrieved 4 July 2017, from https://www.ncbi.nlm.nih.gov/pubmed/26091330
- Burlew CC, e. (2017). Western Trauma Association critical decisions in trauma: resuscitative thoracotomy. - PubMed - NCBI . Ncbi.nlm.nih.gov. Retrieved 4 July 2017, from https://www.ncbi.nlm.nih.gov/pubmed/23188227
- Moore EE, e. (2017). Defining the limits of resuscitative emergency department thoracotomy: a contemporary Western Trauma Association perspective. - PubMed - NCBI . Ncbi.nlm.nih.gov. Retrieved 4 July 2017, from https://www.ncbi.nlm.nih.gov/pubmed/21307731

